- Can I claim OT on private health insurance?
- Do I need a doctor’s referral to see an OT?
- Do you work with children who have NDIS funding?
- How long does therapy continue?
- What happens in the follow-up therapy appointments?
- How can I help my child with drawing and writing?
- How can an Occupational Therapist Help Children?
- How can parents know if their child’s difficulties are significant enough for them to seek help?
- Where is therapy provided?
- What happens at the assessment?
- What is the first step to arrange therapy for your child?
Can I claim OT on private health insurance?
I am registered with most private health insurers and most of them partially cover Occupational Therapy appointment costs on extra cover plans. Please contact your provider for more information regarding this.
Back to Index
Do I need a doctor’s referral to see an OT?
No, you don’t need a doctor’s referral, but some doctors provide a referral letter, which can be helpful. Children who are seeing more than one service provider, e.g. a physiotherapist and an occupational therapist, can often be referred by GPs under a Medicare Chronic Care Plan (or an Enhanced Primary Care Plan). Under these plans, a total five rebates of approximately $50 are available per calendar year for all (but NOT each) of the services.
Children who have a psychological diagnosis e.g. anxiety, autism and ADHD, can be referred to me by GPs or paediatricians under a Mental Health Care Plan. This entitles them to 10 Medicare rebates of approximately $80. If children are also being referred to a psychologist, the total of 10 Medicare rebates is for all services under the plan, not for each service. If you are requesting one of these referrals from your GP, it is important to let the GPs receptionist know that when you make the appointment.
I am registered to provide therapy under both of these types of plans. It is important to note that the rebates do not cover the full cost of the appointments. Payments are usually made at the time of the appointment and EFTPOS facilities are available.
Back to IndexDo you work with children who have NDIS funding?
I provide services to children who have NDIS the funding, and I charge the usual NDIS hourly rate. I do not charge additional amounts for writing regular therapy progress notes, sending emails or making brief phone calls, but I do charge a one hour fee for initial assessment reports and a 30-45 minute fee for review reports.
NDIS currently permits services to charge for appointments which have been missed or cancelled at very short notice.
Families need to self manage their NDIS funding or have a case manager to manage their funding, as I am not registered with NDIS and cannot directly claim payments from NDIS. To find out if your child is eligible for NDIS funding, contact 1800 800 110 or visit www.ndis.gov.au.
Back to IndexHow long does therapy continue?
The number of therapy appointments depends on the severity of difficulties presented. Other considerations include other services that the child is attending, the child’s motivation and insight and the family’s ability to work on goals at home.
Some children only require a few follow-up appointments and some children with significant difficulties require therapy for more than a year.
Back to IndexWhat happens in the follow-up therapy appointments?
At the start of appointments, I write or draw a plan of activities to be undertaken on the day, so everyone knows what we will be doing.
The activities chosen are based on the goals that we have been set, progress that has already been made and input from parents and children.
Activities requiring concentration (e.g. handwriting) are usually alternated with activities that require less concentration and are more energetic (e.g. ball skills). Small rewards including stamps, stickers, sometimes a reward “shop” are offered to provide motivation if necessary.
Back to IndexHow can I help my child with drawing and writing?
- Make sure that your child sits with his/her feet on the floor, at a table which is about 5 cms above elbow height. Encourage him/her to rest both forearms on the table and to sit symmetrically or evenly. Help him/her to be aware of how he/she is sitting by placing your hands on his/her shoulder and head, and asking him/her to feel how he/she is sitting and to try and sit evenly. Encourage your child to tilt his/her work in the same direction as his/her writing forearm (to the left for right handers and to the right for left handers).
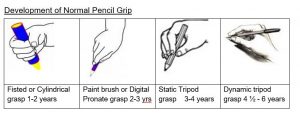
- Encourage your child to hold his/her pencil appropriately for his/her age (see diagram below). Have your child use thick felt pens and pencils at least until he/she starts school. Thin (standard) ones can encourage tight and awkward grips. If your child likes to use your biros, try using thick four-coloured pens. “The pencil grip” is a pencil grip designed to help children become accustomed to holding their pencil using a tripod grasp. The grips can easily be purchased on line.
If your child leans too far forward, or holds his/her pencil in a very upright position (instead of sloping towards their shoulder) place his/her work on a sloping surface. A sloping surface can be easily made or purchased from Plastic Creations in Philip, ACT. An A4 folder has the correct amount of slope and can provide such a surface, though it is a bit small. A sloping surface also helps children to work with their wrist fairly straight and with their hand under the drawing, instead of working with a bent wrist and their hand on top of their work.
- Drawing and writing on a white board, blackboard or some other vertical surface, also helps young children to develop an appropriate grasp, with a straight wrist.
- If your child is in preschool and old enough to start writing his/her name, write their name in large letters, approximately 3cms high, on lines, 3-4 times on a page. After the initial capital letter, use lower case letters, and draw dots and arrows on the letters to indicate the correct way of writing the letters. Place the page in a plastic sleeve and have your child trace over the letters using a whiteboard marker, which can be easily erased.
How can an Occupational Therapist Help Children?
Occupational Therapists are trained to know and understand many aspects of child development, especially the normal order in which skills emerge and the components of each skill. For example, we all know that crawling usually occurs before walking. It is also helpful to know that the ability to transfer weight from one leg to another in turn is important in learning to walk and that this is one of the skills learnt to enable walking to develop. Occupational therapists use this knowledge of developmental pathways to teach skills step by step. These developmental pathways apply to play, social, self-help, thinking and pencil skills as well as to motor skills.
Back to IndexHow can parents know if their child’s difficulties are significant enough for them to seek help?
Many parents find it difficult to know if their child’s problems are really significant, or if they should seek help. It is especially hard if children are embarrassed when their problems become the focus of attention, and if they try to avoid any help that is offered. Embarrassment and avoidance of help often increase with age, so it is advisable to try to decide if help is needed as soon as possible.
I suggest that parents ask themselves the following questions to help them decide if their child would benefit from extra help, including Occupational Therapy.
- How does your child’s level of skills compare with that of other children of the same age? To answer this question, compare him/her with several children, not just one or two. As well, ask teacher, friends and relatives what they think. As a parent myself, I know it is almost impossible to be objective about one’s own children.
- Does your child have difficulty with just one or two skills or with several skills? Of course, problems are more significant if they are widespread than if they just occur with one or two skills. Also, ask yourself whether the skills are important or relatively trivial. Most of use can live happily without being able to play chess, but we would have trouble if we couldn’t tie our shoelaces or write.
- How successful have your attempts been to help him/her with his/her skills? Most parents try to help their children when they have difficulties with skills. If they continue to have difficulty despite your help, they may need help from someone else.
- Is your child developing many secondary effects as a result of his/her difficulties? These may include diminished self-confidence, feeling they are “dumb”, and trying to avoid difficult tasks by withdrawing or misbehaving.
Information about some typical developmental milestones can be found at the Child Development Institute.
It is important that parents and children do not feel that there is some sort of stigma attached to asking for help, or that needing help is proof that they are “dumb”. None of us is good at everything. If a child’s difficulties are preventing him/her from reaching his/her potential, then it may be worth seeking help.
Back to IndexWhere is therapy provided?
Most therapy is provided in my rooms, though occasional, one-off appointments are provided in schools or at home, especially to facilitate liaison with school staff and activities at home.
Parent feedback has indicated that therapy in my rooms is free from the distractions of home and school, and that children often focus at my clinic because they know that this is what is expected. Parents also don’t need to pay for travel time.
Sometimes regular therapy at home and school is the best option for children. Then I suggest that parents seek other therapy providers.
I have now developed a telehealth option for children who are able to utilise on line appointments using Zoom. This option can be used when children or members of their have Covid or other health conditions but are still well enough to engage in therapy. I sometimes use this option for older children who live a considerable distance from my therapy rooms.
Back to IndexWhat happens at the assessment?
At the beginning of the appointment, I explain what we are going to do and make a picture or word plan about the activities. The activities chosen are based on the concerns noted by parents, teachers and children, and developmentally appropriate skills.
At the end of the assessment, we set some goals, and work out some appointment times. Follow up appointments usually last an hour and are usually scheduled approximately once per fortnight. I send an assessment report to parents within a week of the assessment appointment.
Back to IndexWhat is the first step to arrange therapy for your child?
Phone me, Sheila, on (02) 6299 1218. I will discuss your concerns about your child and make a time for an assessment appointment in my rooms, which usually takes 2 hours. I will give you details about my costs and send you a parent questionnaire to fill in and bring to the appointment. I may also send you a teacher questionnaire and/or a sensory questionnaire. Sometimes I make some recommendations that you can start on before your appointment is scheduled.
Back to Index